Radiation exposure during pregnancy is a significant concern due to its potential to harm both the developing fetus and the pregnant individual. The safety of radiation exposure depends on several factors, including the type of radiation, the amount of exposure, and the stage of pregnancy. While radiation has medical uses in imaging (like X-rays, CT scans, and nuclear medicine) and therapeutic settings, precautions must be taken to minimize the risks to the fetus.
Overview of Radiation Risks during Pregnancy
Radiation is classified into two main categories:
- Ionizing radiation: This is the type of radiation most commonly used in medical imaging and therapy (e.g., X-rays, CT scans, radiation therapy). It has enough energy to remove electrons from atoms, potentially causing biological damage.
- Non-ionizing radiation: Examples include radio waves, visible light, and microwaves, which do not have enough energy to cause direct damage to the atoms or cells and are considered much less harmful.
Ionizing radiation is a concern for pregnant individuals, especially during the first trimester when fetal development is at its most vulnerable stage. The fetus, particularly in early pregnancy, is more sensitive to radiation because its cells are dividing rapidly and its DNA is more susceptible to damage.
Types of Radiation and Risks
- X-rays and CT scans:
- These are common imaging techniques that use ionizing radiation. CT scans, in particular, deliver higher doses of radiation than standard X-rays.
- First trimester: The developing fetus is most susceptible to radiation during the first trimester when organogenesis (organ formation) is occurring. Even small doses can lead to developmental defects or miscarriage.
- Later stages of pregnancy: The fetus is less sensitive to radiation later in pregnancy, but exposure can still affect growth or cause other health issues.
- Nuclear Medicine:
- Nuclear imaging techniques use radioactive substances that emit gamma rays. These can pose a higher risk to the fetus, especially if the radioactive substance crosses the placenta. The risk depends on the type of isotope used, the amount of radiation, and the timing of the exposure.
- Teratogenic effects (birth defects), fetal growth restriction, or developmental delays may result from exposure during pregnancy.
- Radiation Therapy:
- Therapeutic radiation is typically not used during pregnancy unless absolutely necessary due to its high doses. It can cause miscarriage, birth defects, or developmental delays in the fetus.
- If radiation therapy is required (for example, in cancer treatment), it is often recommended to delay the treatment or adjust techniques to minimize fetal exposure.
Risks of Radiation Exposure to the Fetus
- Miscarriage: Exposure to high doses of radiation, especially in the early stages of pregnancy, can increase the risk of miscarriage.
- Congenital abnormalities: High doses of radiation during the first trimester can cause malformations of organs and body structures. The critical period for this risk is from conception to about 8 weeks of gestation.
- Developmental delays: Exposure to radiation can affect the brain and nervous system, leading to intellectual disabilities, motor deficits, and other developmental issues. The risk is highest if the exposure occurs between 8 and 15 weeks of pregnancy.
- Cancer risk: Long-term effects include an increased risk of childhood cancers, especially leukemia and brain tumors. This risk is dose-dependent and higher with early exposure.
Guidelines for Radiation Exposure during Pregnancy
General Recommendations:
- Minimize exposure: The goal is to limit unnecessary radiation exposure during pregnancy. For any medical procedure involving radiation, the risks should always be weighed against the potential benefits.
- Use of alternative methods: Non-radiation imaging techniques, such as ultrasound or MRI, should be preferred over X-rays or CT scans if they provide the necessary diagnostic information.
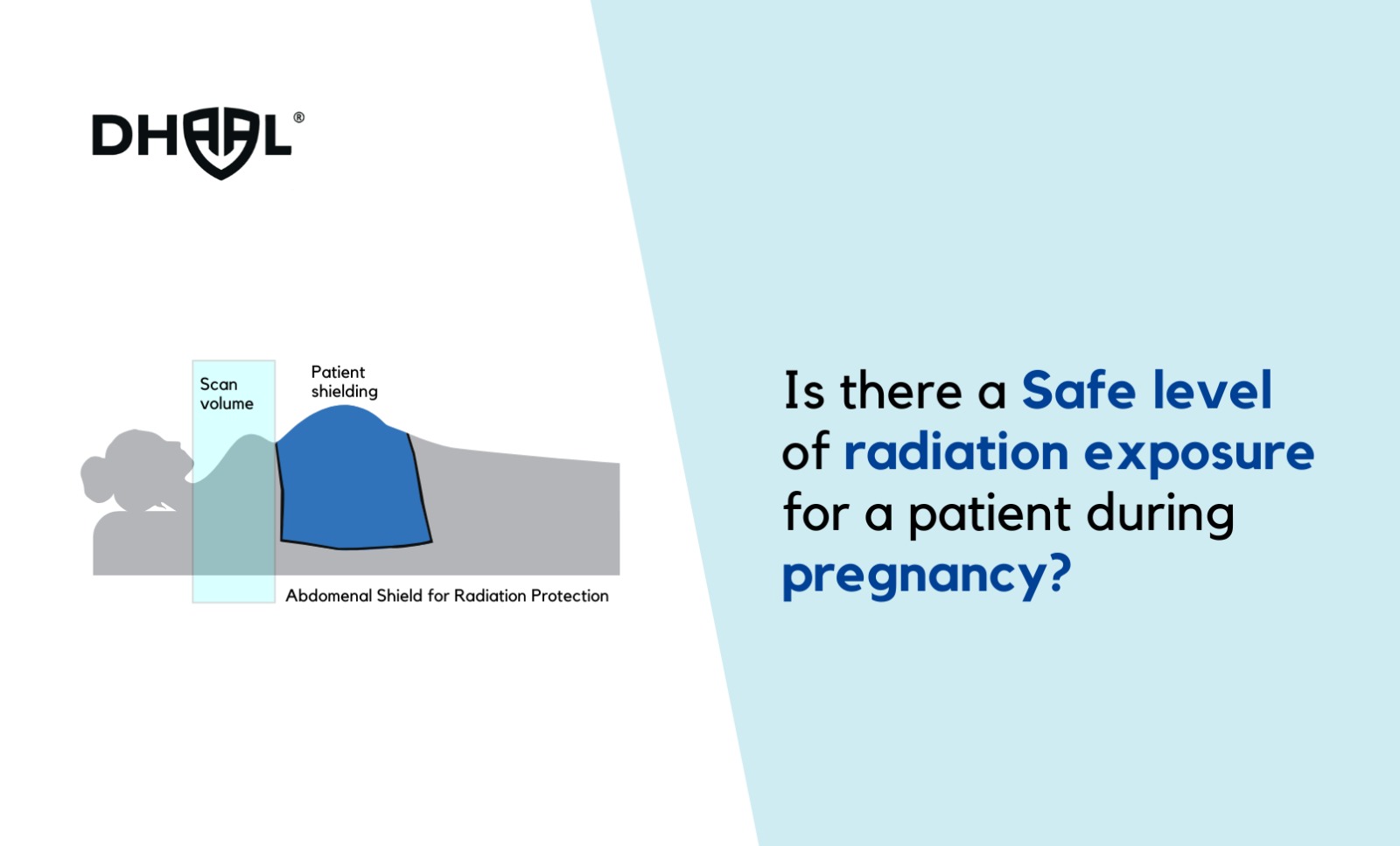
- Fetal shielding: In certain cases, lead shielding can be used to protect the abdomen during X-ray or CT imaging, although its effectiveness for protecting the fetus is limited.
- Dosage guidelines: The National Council on Radiation Protection and Measurements (NCRP) recommends that radiation exposure to the fetus should not exceed 5 millisieverts (mSv) for the entire pregnancy. This is based on the understanding that doses below this level are unlikely to result in significant harm.
Pregnancy Stages and Radiation Sensitivity:
- Preconception and Early Pregnancy (0–2 weeks): The risk of radiation during this stage is primarily related to the possibility of miscarriage. The embryo is most susceptible to lethal doses of radiation, but radiation exposure during the very early stages may not lead to birth defects because the embryo has not yet developed organs.
- Organogenesis (2–8 weeks): This is the most critical period for radiation exposure, as this is when the organs and major structures are forming. Exposure to high doses can lead to congenital defects or developmental abnormalities.
- Fetal Growth and Development (8 weeks–birth): The risk of birth defects declines, but exposure to radiation during this stage can still cause growth restrictions or impact neurological development, particularly in the brain.
Diagnostic and Therapeutic Procedures: Considerations for Pregnant Patients
- X-ray and CT scans:
- X-rays: When medically necessary, an X-ray may be performed with the abdomen shielded. It is generally considered safe if the exposure is minimal and if the benefits outweigh the risks.
- CT scans: Because CT scans involve higher radiation doses, they should be avoided during pregnancy unless absolutely necessary. If a CT scan is required, efforts should be made to reduce the radiation dose, such as limiting the area scanned.
- MRI and Ultrasound:
- These modalities do not use ionizing radiation and are generally considered safe during pregnancy. MRI is particularly useful for soft tissue imaging, and ultrasound is widely used for fetal monitoring and diagnosis.
- Nuclear Medicine:
- This should be avoided during pregnancy unless it is crucial for diagnosis and there are no alternative options. If it is performed, the radiation exposure should be minimized and considered only when the potential benefit outweighs the risks.
Conclusion
There is no “safe” level of radiation exposure during pregnancy, but the goal is to keep exposure to a minimum. The potential risks to the developing fetus, such as miscarriage, birth defects, developmental delays, and cancer, must be carefully considered against the benefits of the medical procedure. In most cases, non-radiation imaging methods like ultrasound or MRI are preferred, and radiation should only be used when absolutely necessary. If radiation exposure is unavoidable, careful consideration of the dose, timing, and type of radiation, along with proper shielding and protection, can help reduce risks. The healthcare team must provide informed counseling to pregnant patients about the potential risks and alternatives before proceeding with radiation-based procedures.